We are the only charity in the UK dedicated to funding hearing research. Since 2000, we have funded over £28 million of research and supported 443 ground-breaking projects around the world – and we’re not done yet.
What we’re funding now
Explore our three areas of research focus: restoring hearing, silencing tinnitus, and preventing hearing loss.
Are you seeking funding opportunities for your research? Apply for funding now.

The impact of our research
About our research
We’re working towards a future where treatments and cures for hearing loss and tinnitus exist for those who want them. This is how we’re making that happen.
Keep up with the latest research
Stay up to date with developments in the field by signing up to our monthly charity newsletter or keeping an eye on hearing research clinical trials happening around the world.
“At home I can have my kids on either side of me when we are having a conversation or watching TV. When we are in the car, I can hear whoever is in the passenger seat or back, which is huge because I’ve never been able to do that before.”
Shakib, hearing aid user. Read Shakib’s story.


Support life-changing research
For researchers
We support established researchers and those at the beginning of their careers.
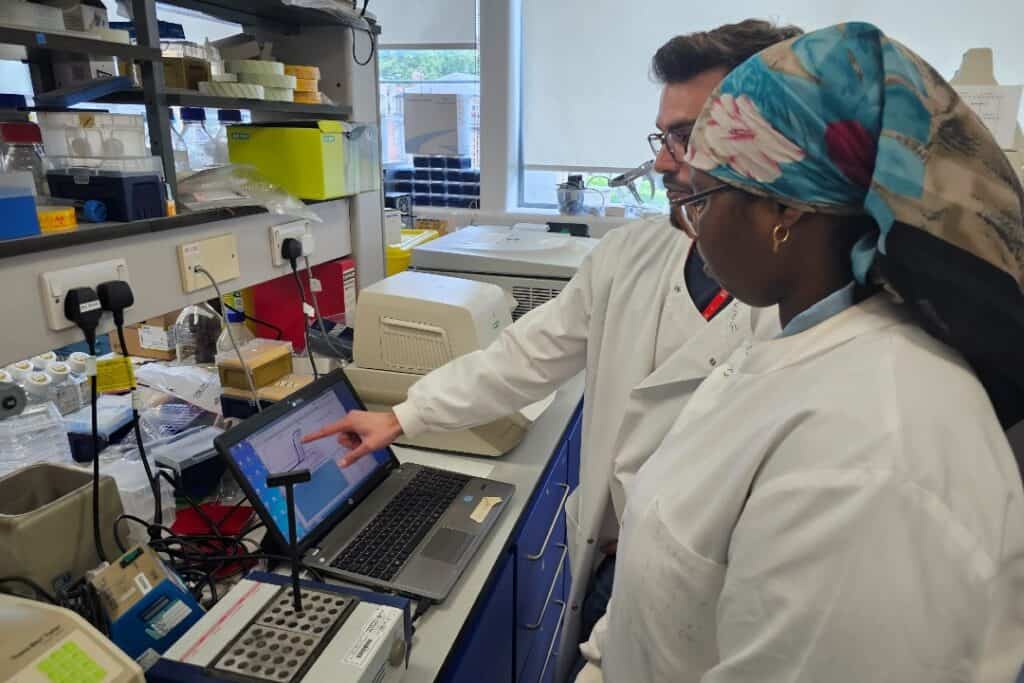
Through Fellowships for post-PhD researchers, PhD studentships and summer placements as part of In2scienceUK’s In2research scheme, we’re fighting the barriers that can bar entry into hearing research.
Working with my host was wonderful as he was always open to answering my questions and ensuring I understood the research. Through this experience, I not only gained vital practical skills, but also an understanding of the day-to-day working life of a researcher.”
Nuura Ahmed, In2scienceUK RNID funding awardee.
Apply for research funding
Through our Discovery Research Grants and Translational Research Grants, we support research to underpin and drive forward the development of new treatments for hearing loss and tinnitus. And our Innovation Seed Fund supports brand new ideas that need funding to get started.
Discover opportunities to apply for grants and funding from RNID.